Clinical Journal of Pain:
POST AUTHOR CORRECTIONS, 20 December 2010
doi: 10.1097/AJP.0b013e31820215f5
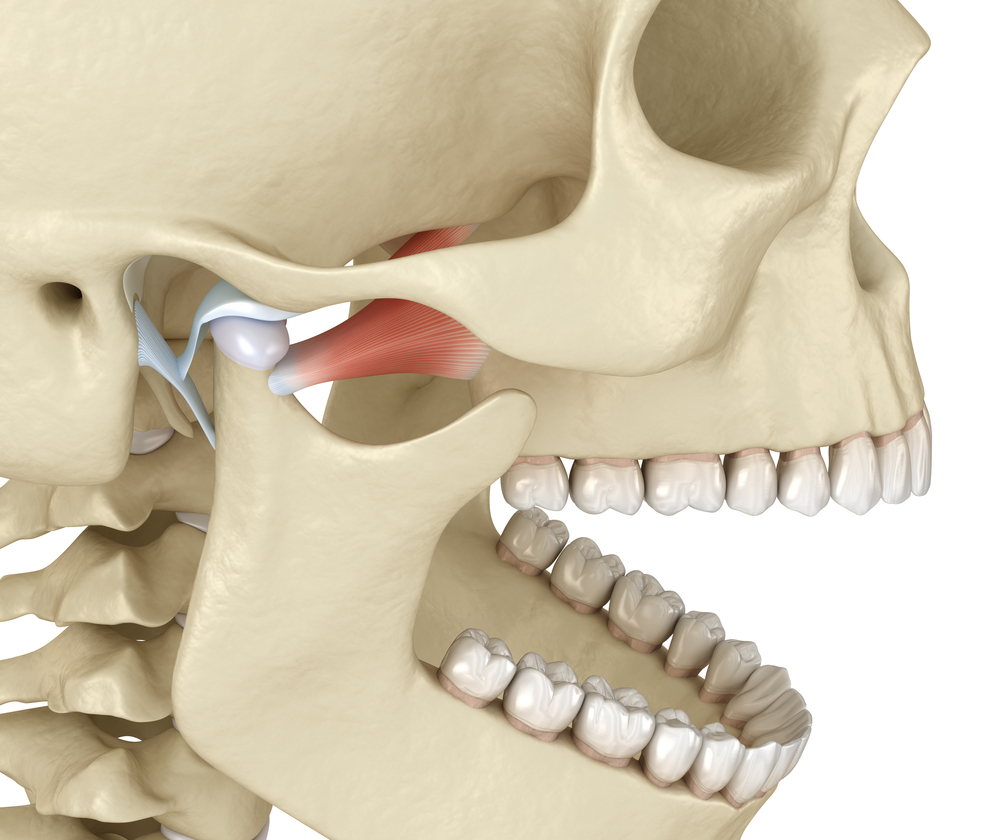
Temporomandibular Disorders and Associated Clinical Comorbidities
Abstract Objective: Temporomandibular joint and muscle disorders (TMJD) are ill-defined, painful debilitating disorders. This study was undertaken to identify the spectrum of clinical manifestations based on self-report from affected patients.
Methods: A total of 1511 TMJD-affected individuals were recruited through the web-based registry of patients maintained by The TMJ Association, Ltd, a patient advocacy organization, and participated in the survey as well as 57 of their nonaffected friends. Results were also compared with US population for questions in common with the National Health and Nutrition Examination Survey.
Results: The TMJD-affected individuals were on average 41 years of age and predominantly female (90%). Nearly 60% of both men and women reported recent pain of moderate-to-severe intensity with a quarter of them indicating interference or termination of work-related activities. In the case-control comparison, a higher frequency of headaches, allergies, depression, fatigue, degenerative arthritis, fibromyalgia, autoimmune disorders, sleep apnea, and gastrointestinal complaints were prevalent among those affected with TMJD. Many of the associated comorbid conditions were over 6 times more likely to occur after TMJD was diagnosed. Among a wide array of treatments used (46 listed), the most effective relief for most affected individuals (91%) was the use of thermal therapies-hot/cold packs to the jaw area or hot baths. Nearly 40% of individuals affected with TMJD patients reported one or more surgical procedures and nearly all were treated with one or many different medications. Results of these treatments were generally equivocal. Although potentially limited to the most severe TMJD affected individuals, the survey results provide a comprehensive dataset describing the clinical manifestations of TMJD.
Discussion: The data provide evidence that TMJD represent a spectrum of disorders with varying pathophysiologies, clinical manifestations, and associated comorbid conditions. The findings underscore the complex nature of TMJD, the need for more extensive interdisciplinary basic and clinical research, and the development of outcome-based strategies to more effectively diagnose, prevent, and treat these chronic, debilitating conditions.
(C) 2010 Lippincott Williams & Wilkins, Inc.
Also, according to an article posted at www.Fibromyalgia-Symptoms.org, 75% of fibromyalgia sufferers also have TMJ / TMD, or Temporal Mandibular Joint Dysfunction.
In May of 2007, the Orofacial Pain Center of the University of Kentucky in Lexington (rbalasub@dental.upenn.edu) published the results of a study comparing the prevalence of temporomandibular disorders in fibromyalgia and “failed back syndrome” patients. 53% of the Fibromyalgia patients reported having face pain compared with 11% of the FBS patients. Of those Fibromyalgia patients who reported face pain, 71% fulfilled the criteria for a diagnosable TMD.
Dr. Stan Farrell, AZ TMJ and his sister Dr. Estelle Farrell, Arizona PM&R are working closely together to help patients find relief for many of these comorbidities. Dr. Farrell focuses on conservative treatments, without the use of narcotics or surgical procedures. www.headpaininstitute.com