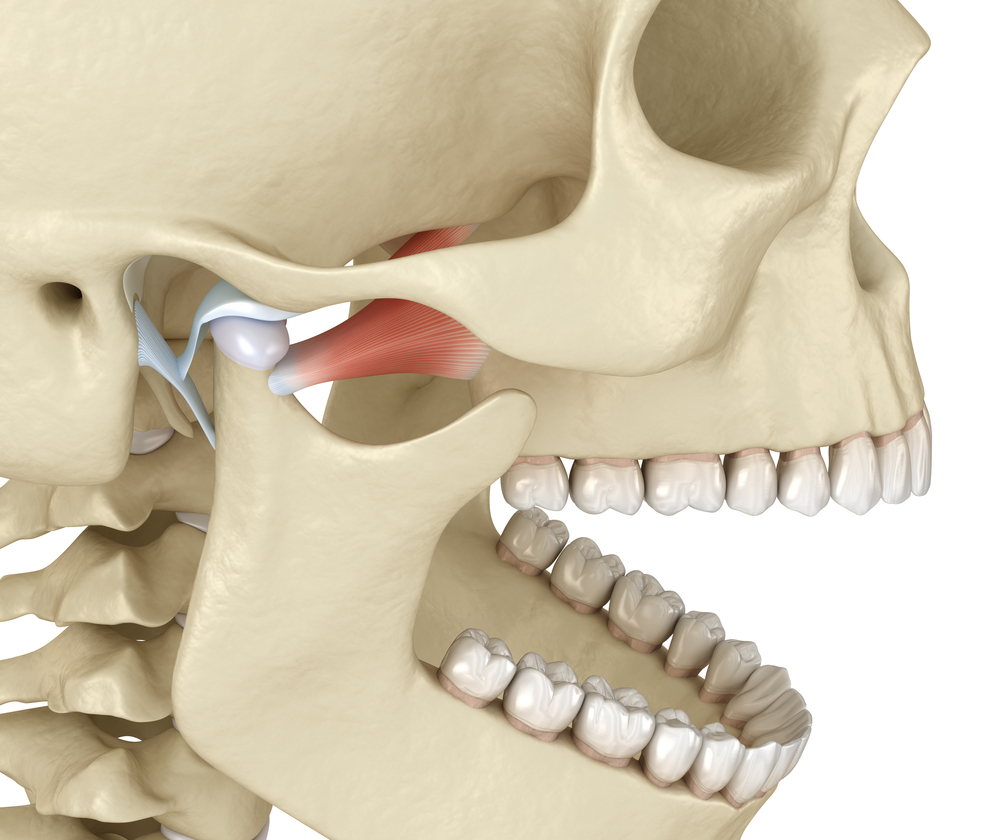
How important is cone-beam computed tomographic (CT) images in the diagnosis of temporomandibular joint disorders (TMD)? A new 2014 study conducted by the Department of Oral and Maxillofacial Surgery, University of Groningen, The Netherlands aimed to assess the value of these CT images. Oral and maxillofacial surgeon’s, specialists, and residents examined 128 outpatients with TMD disorders. After diagnosis and treatment plans were established, the physicians reviewed the cone-beam CT images. After reviewing the images, they changed the diagnosis and treatment plans in more than half of the patients with TMJ disorders. Dr. Stan Farrell is a Diplomate with the American Board of Orofacial Pain, making him one of the best choices for your temporomandibular pain treatment. He uses the latest technology in imaging to accurately diagnose TMD issues in the joint with every patient. If you or someone you know suffers from joint pain or muscle pain, please contact Dr. Stan Farrell at 480-945-3629 or at www.aztmj.com to schedule a consultation.
de Boer EW1, Dijkstra PU2, Stegenga B3, de Bont LG3, Spijkervet FK3. Department of Oral and Maxillofacial Surgery, University of Groningen, University Medical Centre Groningen, Groningen, The Netherlands.
Abstract: The objective of this study was to assess the value of cone-beam computed tomographic (CT) images in the primary diagnosis and management of 128 outpatients with disorders of the temporomandibular joint (TMJ). Before a diagnosis was made and treatment planned, the history was taken, physical examination made, and the orthopantomogram studied. After assessment of the cone-beam CT, the oral and maxillofacial surgeon (specialist or resident) was allowed to revise the provisional primary diagnosis and management. The degree of certainty was rated by the clinician before and after the cone-beam CT had been assessed. The primary diagnosis was changed in 32 patients (25%), additional diagnostic procedures were changed in 57 (45%), and the treatment was changed in 15 (12%) (in 4 the treatment was changed to a (minimally) invasive procedure). A total of 74 patients (58%) had their diagnosis and management changed after the cone-beam CT had been assessed. Changes in diagnosis and management were clinically relevant in 9/32 and 9/61 patients, respectively. The clinician’s certainty about the primary diagnosis increased after the cone-beam CT had been assessed in 57 patients. Logistic regression analysis showed that the odds in favor of changes in primary diagnosis and management increased when limited mandibular function was a primary symptom, the patient was taking medication for pain, and the articular eminence could not be assessed on OPT. Assessment of cone-beam CT led to changes in primary diagnosis and management in more than half the patients with disorders of the TMJ.