Orofacial Pain
The emerging specialty of Orofacial Pain Dentistry is concerned with the prevention, evaluation, diagnosis, treatment, and rehabilitation of orofacial pain disorders. Such disorders may have pain and associated symptoms arising from a discrete cause, such as postoperative pain or pain associated with a malignancy, or may be syndromes in which pain constitutes the primary problem, such as neuropathic pains or headaches. The orofacial pain dentist serves as a consultant to other dentists and physicians but is often the principal treating health care provider and may provide care at various levels, such as direct treatment, prescribing medication, prescribing rehabilitative services, performing pain relieving procedures, counseling of patients and families, direction of a multidisciplinary team, coordination of care with other healthcare providers and consultative services to public and private agencies pursuant to optimal healthcare delivery to the patient suffering from a painful disorder.
Exam
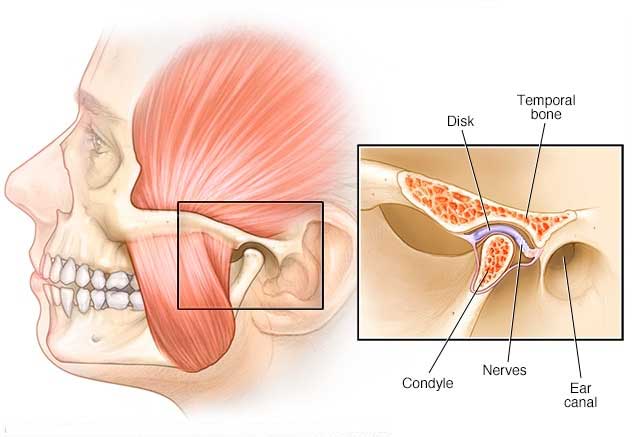
Patients can expect a thorough evaluation of musculoskeletal and nerve functions of TMJ, head and neck palpations, headache / migraine trigger points, measuring opening/side to side, use of MRI or CT images to accurately diagnose TMD issues, listening to joint sounds for arthritis / crepitus, and evaluation of medication use.
Treatments
Occlusal Orthotic: It may be recommended that you wear an orthotic (also known as a splint-different from a night guard or bite guard) that fits over either your upper or lower teeth. An orthotic has many different uses and can be worn either full time or part time, depending what your doctor determines is best for you. Generally, orthotics are used to keep the teeth apart, realign the jaw joints and help the jaw muscles relax. The specific design and adjustment of your orthotic will depend upon your condition, how it changes during the time you wear your orthotic, and your overall treatment plan.
Trigger Point Injections: Many headaches, migraines and facial pain can be pinpointed to a specific trigger point, either a muscle or nerve. By injecting the muscle with medication, the headache and other pain triggers are blocked.
Joint Injections: Injections into the TMJ joints, usually includes steroid with anesthetic, to lubricate and relieve pain from joints.
Nerve Blocks: Occipital and trigeminal blocks with steroid and anesthetic to diagnose or eliminate pain.
Stress Management: One treatment approach for your TMD problem is to learn to manage your daily stress. Your doctor may recommend several techniques to help you do this. They may include biofeedback, relaxation breathing, guided imagery, and sometimes referral to a therapist.
Physical Therapy: Physical therapists are trained professionals who help rehabilitate all types of physical injuries. There are many different techniques that are helpful and the most common include jaw exercises, postural and ergonomic training, ultrasound, electrical stimulation, and mobilization. Your doctor and physical therapist will work together to formulate a plan for your treatment.
Extensive research is being conducted on the safety and effectiveness of TMD/orofacial pain treatments. Most researchers and clinicians strongly recommend reversible and conservative treatments for TMD. Even when TMD symptoms are long standing and severe, most TMD patients do not require invasive treatment. Treatments designed to permanently change the bite or reposition the jaw with orthodontics or dental reconstruction are not usually necessary and should be undertaken with great care.
If irreversible treatment (permanent change) for TMD or orofacial pain is contemplated, we recommend getting a reliable second opinion.
Specially trained dentists, physical therapists, psychologists and physicians are usually the best source for the proper diagnosis and management of TMD and Orofacial pain.
See how our Orofacial Pain treatment compares to the cost and methods of other treatment options.
Results and Research
Temporomandibular disorder symptoms are more common in migraine, episodic headache, and chronic daily headache relative to individuals without headache. Magnitude of association is higher for migraine. Future studies should clarify the nature of the relationship. — Headache and Symptoms of Temporomandibular Disorder: An Epidemiological Study OnabotulinumtoxinA (Botox; Allergan Brand) has now been FDA approved for the treatment of migraine headaches. OnabotulinumtoxinA (Botox) has been reported to relieve pain in a variety of conditions, including migraine headaches. In a recent study in Headache Journal of Head and Face Pain, 89% of patients with episodic migraine who were treated with OnabotulinumtoxinA had complete or partial response of their migraine symptoms, including headache. Treatment of temporomandibular disorders by stabilizing splints in general dental practice: results after initial treatment. — Method of Injection of Botox of Chronic Migraine is Safe and Effective Treatment “80% TMD patients were managed effectively by using splints for periods of up to five months.” “When interested and suitably trained, general dental practitioners can manage four out of five TMD patients with reversible treatment in their own practices.” — Medical treatment of recurrent temporomandibular joint dislocation using botulinum toxin A

