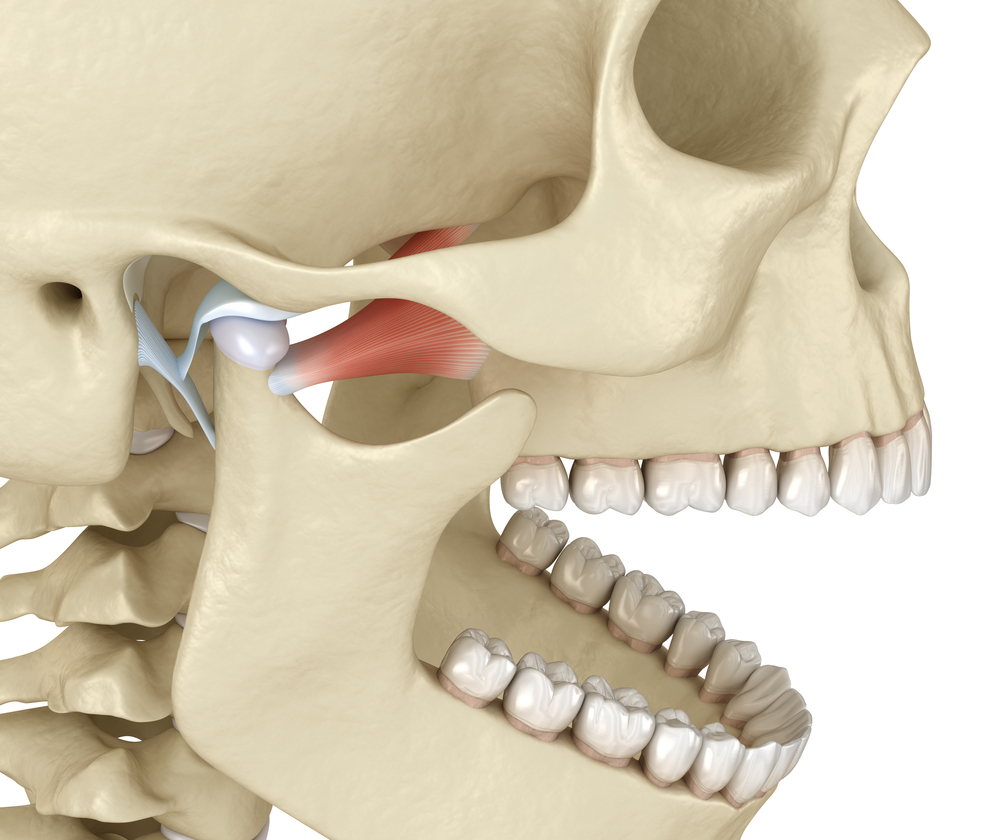
A recent study was conducted to investigate the association among temporomandibular disorders (TMD), sleep bruxism, and primary headaches, assessing the risk of occurrence of primary headaches in patients with or without painful TMD and sleep bruxism. 301 individuals participated in the study (253 women and 48 men), with the average age being 37.5 years. An association was found among tension-type headache, painful TMD, and migraine headache. The association of painful TMD and sleep bruxism considerably increased the risk for tension-type headache, migraine, and especially for chronic migraine. Dr. Stan Farrell, whose office is located in Scottsdale, Arizona, focuses on the treatment of all types of headaches, especially migraines. Dr. Farrell is Board Certified and a member of the American Headache Society and a Diplomate with the American Board of Orofacial Pain, making him one of the best choices for your migraine headache treatment. If you suffer or know someone who suffers from migraines or headaches, schedule an appointment with Dr. Farrell at AZ TMJ today. www.headpaininstitute.com
J Orofac Pain. 2013 Winter;27(1):14-20. doi: 10.11607/jop.921.
Temporomandibular disorders, sleep bruxism, and primary headaches are mutually associated.
Fernandes G, Franco AL, Gonçalves DA, Speciali JG, Bigal ME, Camparis CM.
Abstract:
Aims: To investigate the association among temporomandibular disorders (TMD), sleep bruxism, and primary headaches, assessing the risk of occurrence of primary headaches in patients with or without painful TMD and sleep bruxism. Methods: The sample consisted of 301 individuals (253 women and 48 men) with ages varying from 18 to 76 years old (average age of 37.5 years). The Research Diagnostic Criteria for Temporomandibular Disorders were used to classify TMD. Sleep bruxism was diagnosed by clinical criteria proposed by the American Academy of Sleep Medicine, and primary headaches were diagnosed according to the International Classification of Headache Disorders-II. Data were analyzed by chi-square and odds ratio tests with a 95% confidence interval, and the significance level adopted was .05. Results: An association was found among painful TMD, migraine, and tension-type headache (P < .01). The magnitude of association was higher for chronic migraine (odds ratio = 95.9; 95% confidence intervals = 12.51-734.64), followed by episodic migraine (7.0; 3.45-14.22) and episodic tension-type headache (3.7; 1.59-8.75). With regard to sleep bruxism, the association was significant only for chronic migraine (3.8; 1.83-7.84). When the sample was stratified by the presence of sleep bruxism and painful TMD, only the presence of sleep bruxism did not increase the risk for any type of headache. The presence of painful TMD without sleep bruxism significantly increased the risk in particular for chronic migraine (30.1; 3.58-252.81), followed by episodic migraine (3.7; 1.46-9.16). The association between painful TMD and sleep bruxism significantly increased the risk for chronic migraine (87.1; 10.79-702.18), followed by episodic migraine (6.7; 2.79-15.98) and episodic tension-type headache (3.8; 1.38-10.69). Conclusion: The association of sleep bruxism and painful TMD greatly increased the risk for episodic migraine, episodic tension-type headache, and especially for chronic migraine. J OROFAC PAIN 2013;27:14-20.