December 13, 2010
The New York Times
Narcotic Painkillers May Pose Danger to Elderly Patients, Study Says By BARRY MEIER
Older patients with arthritis who take narcotic-based drugs to relieve pain face a higher risk of bone fracture, heart attack and death when compared to those taking non-narcotic drugs, according to a government-financed study published Monday.
The study, in The Archives of Internal Medicine, appears to be the first large-scale effort to look at the comparative safety risks for the elderly taking different classes of painkillers. The use of narcotic painkillers has increased in recent years because of a prevailing belief that such drugs were safer for older patients than non-narcotic drugs like Advil and Motrin.
The review, financed by the federal Agency for Healthcare Quality and Research, appears to undercut that assumption. The report, which was based on an analysis of patient health care records, was conducted by researchers at Brigham and Womens Hospital in Boston.
“Doctors should not assume that opioids are a safer alternative,” to other painkillers, said Daniel H. Solomon, the study’s researcher, said in a telephone interview on Monday. “They seem to carry profound risks to cardiovascular system as well as increased risk fractures and appear to be associated with increased risk of death.”
The study does not raise questions about the use of powerful narcotics like OxyContin to treat severe pain resulting from cancer or other conditions.
To conduct the study, Dr. Solomon reviewed the experience of Medicare recipients in both New Jersey and Pennsylvania who were found during a six-year period to have osteoarthritis or rheumatoid arthritis. Using statistical methods, researchers divided those patients, predominantly women with a mean age of 80 years, into three groups based on their pain medications.
Patients in one group received a narcotic-based painkiller. The second group took a non steroidal anti-inflammatory drug like Advil or Aleve. The third group took another class of pain drugs called coxibs, which include Celebrex and Vioxx, a drug that is no longer on the market.
Because the study was based on records, it could not identify all factors that might have contributed to a patient’s problems. But researchers found that the overall risk of death was twice as high for patients taking a narcotic painkiller when compared to those taking a non steroidal anti-inflammatory drug.
More specifically, patients in the narcotic group were four times more likely to experience a compound bone fracture, apparently as a result of a fall, and they were twice as likely to have a heart attack. The cardiovascular risks posed by narcotics were the same as for drugs like Celebrex and Vioxx, which have come under scrutiny for that hazard.
The review also found that the rate of gastrointestinal bleeding among patients taking narcotics was about the same as those taking drugs like Advil and Aleve. A principal reason that medical experts have advocated narcotics in older patients is the belief that they reduce such problems.
In an commentary accompanying the new report, two physicians at Yale University Medical School, Dr. William C. Becker and Dr. Patrick G. O’Connor, wrote that the study’s findings, like those regarding bleeding ulcers, could be skewed by undocumented patient use of over-the-counter painkillers. They added, however, that the high incidence of bone fractures, which often lead to fatal complications in the elderly, were troublesome.
In a related study that was also published Monday in The Archives of Internal Medicine, Dr. Solomon and other researchers looked at the comparative risks posed by different narcotics.
Using the same patient records, they reported that cardiovascular risks were highest for codeine and that codeine and oxycodone, the active ingredient in drugs like OxyContin, posed higher mortality-related risks than hydrocodone, the active ingredient in drugs like Vicodin.
The Food and Drug Administration recently moved to stop sales of one narcotic painkiller, proproxyphene, citing its heart risks. The drug was used in both Darvon and Darvocet.
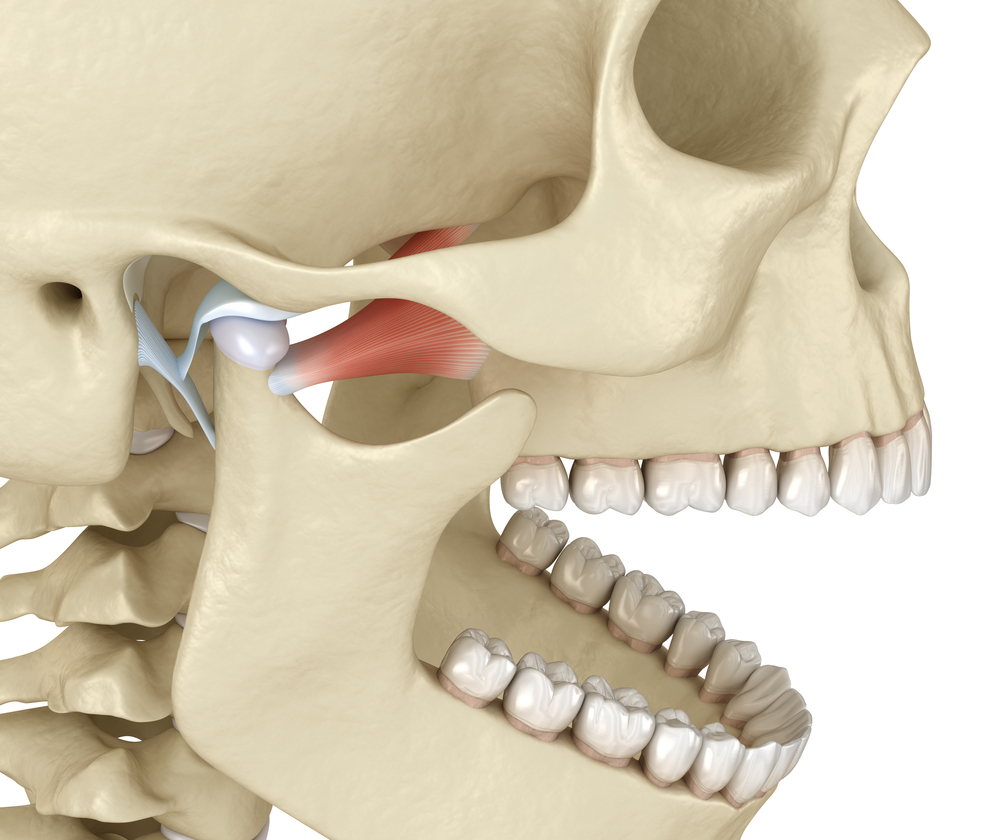
Dr. Stan Farrell, AZ TMJ, focuses on using treatment methods for headache, migraine and TMJ / TMD pain that provide relief without the use of narcotics. https://www.headpaininstitute.com/