What Is TMJ Disorder?
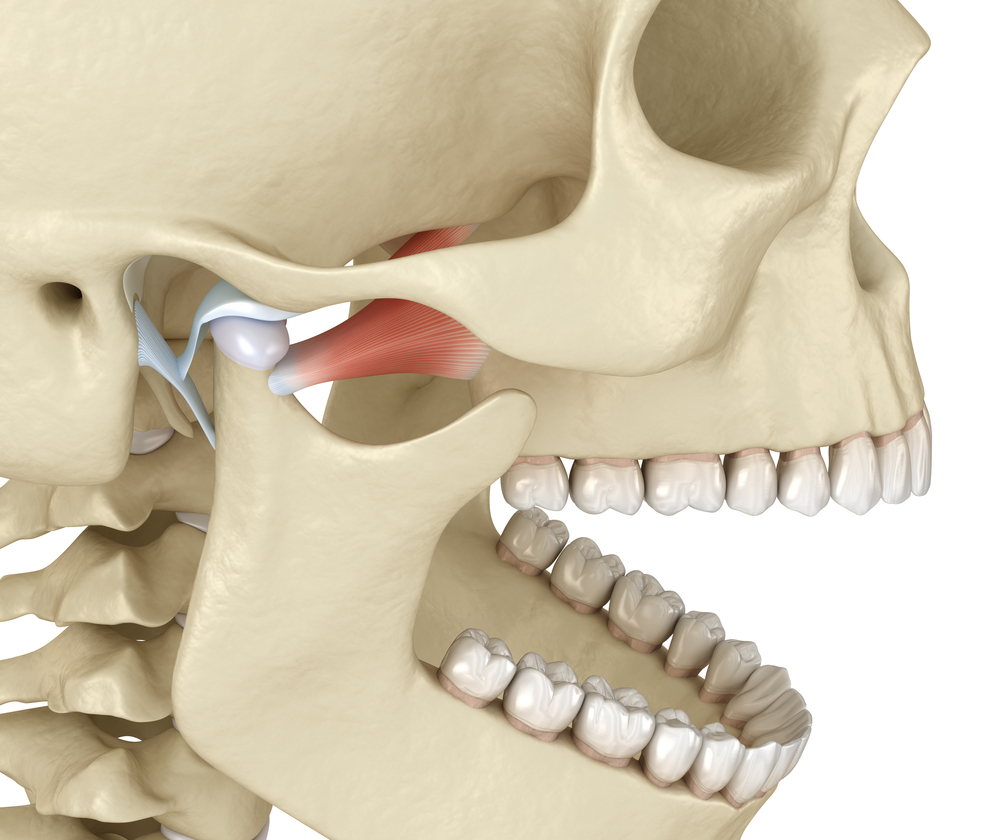
TMJ disorder refers to discomfort and dysfunction of the TMJ and jaw muscles. The discomfort may also spread to the face, neck, and ears. The TMJ is a sliding hinge that joins the mandible to the skull immediately below the ear on either side of the head. It moves up and down, side to side, and back and forth. TMJs, which are always active throughout the day, let us yawn, eat, talk, and do other things with our mouths.
What Is OSA?
The most prevalent kind of sleep apnea is OSA, which is characterized by frequent pauses in breathing during sleep. It is generally accompanied by loud snoring and sudden awakenings with gasping or choking. In extreme situations, this can happen up to 30 times each hour, with breathing paused for 10 seconds or longer.
Breathing is disrupted during sleep when the throat muscles relax too much and obstruct or severely limit the airway. When the brain detects this, the central nervous system is activated, causing breathing to resume. OSA patients frequently awaken temporarily as this occurs, but these awakenings are generally so fleeting that they are not noticed. As a result, a lack of restorative sleep can cause a slew of life-altering or sometimes fatal symptoms.
Cause and Effect
Studies have shown that there is a clear connection between OSA and TMJ disorders. Certain factors may affect the connection between the two conditions. OSA patients, for example, may experience more motor activity in the upper airway muscles when their bodies try to keep their airways open during sleep by pushing the lower jaw forward.
This can lead to teeth clenching and grinding, a condition known as bruxism. It puts strain on the TMJ and its articular disc, as well as the muscles and tissues around it. This pressure and overuse can lead to inflammation and painful TMJ disorders.
In other cases, OSA and TMJ disorders may have the same underlying etiology. Malocclusion, for example, might contribute to OSA development by causing the airway to become closed during sleep. Malocclusion also prevents jaw muscles from resting in an optimal posture, putting tension on the TMJ.
Implications on Screening and Treatment
With studies showing a clear connection between OSA and TMJ disorders, it is important that the method to detect and optimally treat both disorders must incorporate this relationship. When a patient exhibits one or both of these symptoms, optimal practices should involve screening for both. If one is originally present but not the other following examination and diagnosis, such as OSA without TMJ disorders, TMJ disorders screening should be done on a regular basis.