There is a growing trend to use the transcutaneous electrical nerve stimulation (TENS) in the treatment of TMJ/TMD. Dr. Stan Farrell, a Diplomate with the American Board of Orofacial Pain, does not currently use the TENS machine in the treatment of TMJ/TMD because studies showing this device effectiveness in treating TMJ/TMD long-term are limited. While Dr. Farrell does not recommend TENSing his patients, he does employ the latest methods and technology in diagnosing and treating his patients with techniques that are substantiated by significant amounts of documented research. Additionally, the study published in Quintessence International by several leading doctors from Germany present findings that show no significant connections exist between functional occlusion/malocclusion and TMD. These findings challenge neuromuscular dentists who attempt to fix TMJ/TMD through fixing a “bad bite” or malocclusion. Dr. Farrell’s approach and philosophy of treatment is proven and validated by years of advanced study. To set up your consultation contact Dr. Farrell at 480-945-3629. www.headpaininstitute.com
Dietmar Gesch, Dr Med Dent/Olaf Bernhardt, Dr Med Dent/Antje Kirbschus, Dr Med Dent
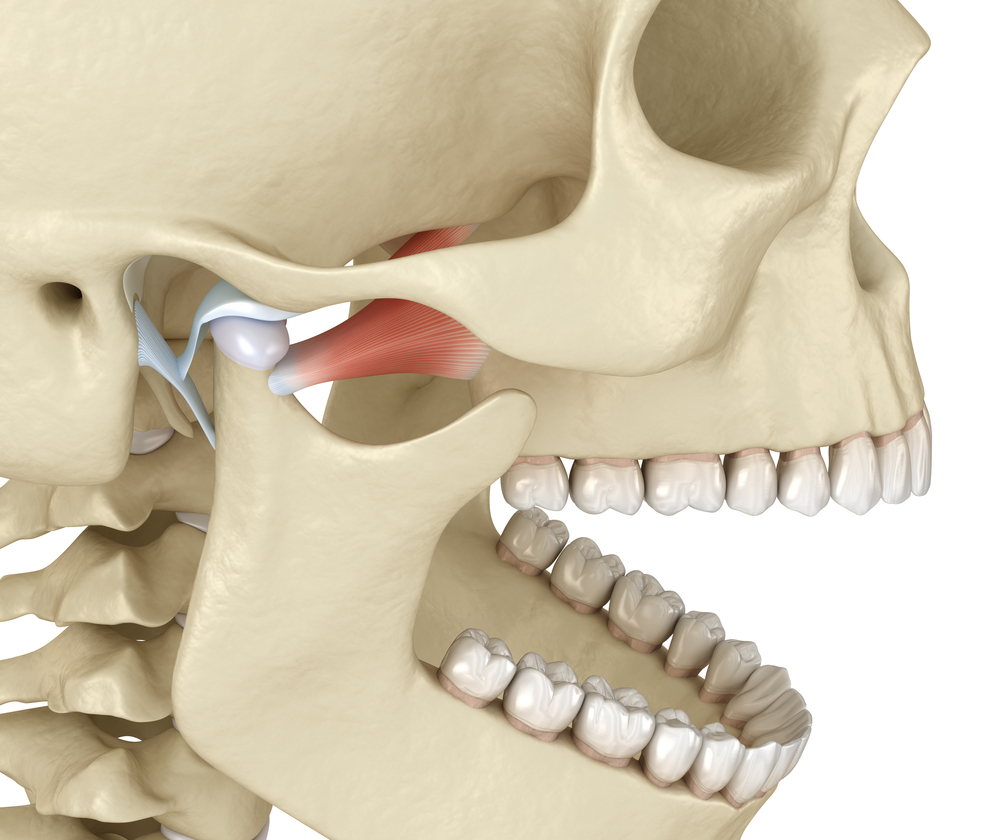
AIM: The aim of this systematic review of population-based studies was to establish whether or not associations exist between different types of malocclusions, as well as factors of functional occlusion (eg, occlusal interferences, nonworking-side occlusal contacts) and temporomandibular disorders (TMD) in adults 20 years or older.
Methods: Defined criteria were employed in the search of MEDLINE and EMBASE databases, as well as in a manual search. Finally, using inclusion criteria (eg, random sampling from residents’ registration office files or census lists, adequate response rates), out of 22 preselected studies, four relevant population-based studies on this subject were found. Eighteen studies were excluded because of insufficient description of material and methods (eg, lack or unclear description of sample method, randomization, age distribution), mixed under- and over-20-year-old study population, or different outcome of interest (eg, tooth loss, dentures). The methodologic quality of the selected studies was established with a quality assessment list.
Results: The average total methodologic score achieved was 43 out of a possible 100 points. Few associations were reported between malocclusion and parameters of functional occlusion and clinical as well as subjective TMD, and these associations were not uniform. No particular morphologic or functional occlusal factor became apparent. Additionally, the occlusal factors found were partly protective for TMD, ie, subjects with these occlusal parameters showed fewer signs and symptoms of TMD (angle Class II malocclusion, deep bite, anterior crossbite). A positive relationship was only described in two cases—between the number of rotated lateral teeth and subjective symptoms of dysfunction, and between excessive abrasions and clinical dysfunction. In neither case, however, was the strength of the correlation given.
Conclusion: In summary, few associations were established between malocclusion or functional occlusion and signs and symptoms of TMD. In view of the small number of randomized studies and their methodologic quality, these results should be verified through further valid representative studies. (PMID: 15119680PG:211-221)