Niloofar Afari, PhD/Yang Wen, MS/Dedra Buchwald, MD/Jack Goldberg, PhD/Octavia Plesh, DDS, MD
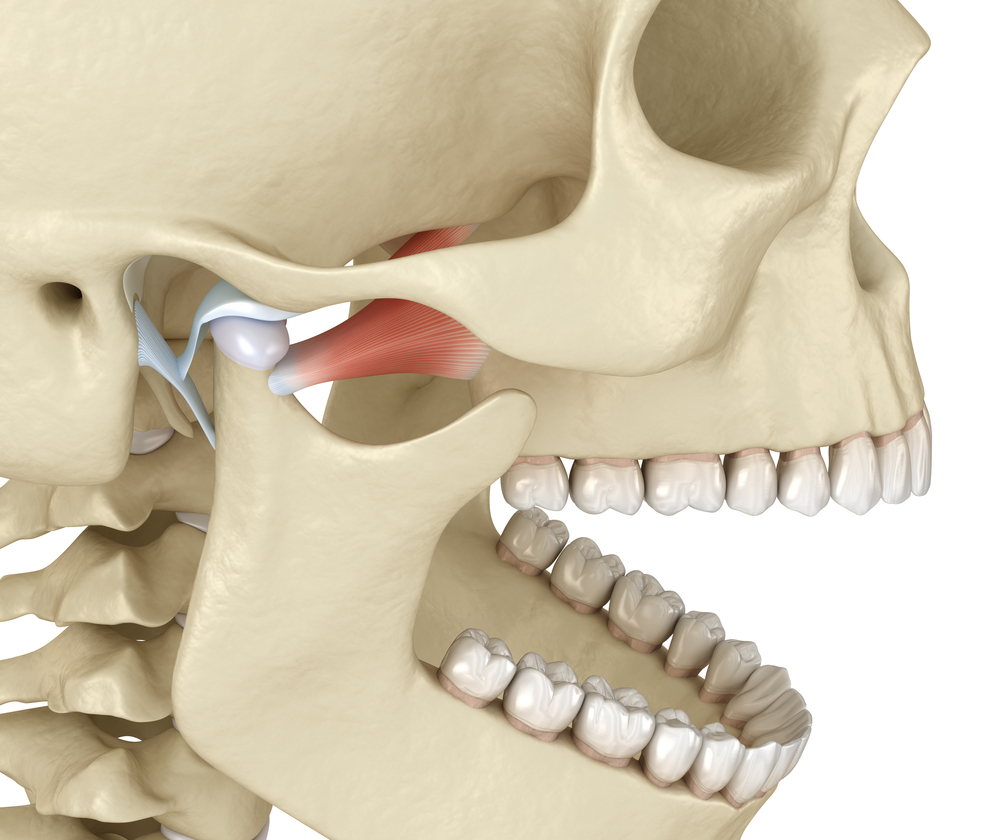
Aims: To determine whether symptoms of post-traumatic stress disorder (PTSD) are related to the pain of temporomandibular disorders (TMD) in a community-based sample of female twin pairs, and if so, to ascertain whether the association is due to the presence of chronic widespread pain (CWP) and familial/genetic factors.
Methods: Data were obtained from 630 monozygotic and 239 dizygotic female twin pairs participating in the University of Washington Twin Registry. PTSD symptoms were assessed with the Impact of Events Scale (IES), with scores partitioned into terciles. TMD pain was assessed with a question about persistent or recurrent pain in the face, jaw, temple; in front of the ear; or in the ear during the past 3 months. CWP was defined as pain located in 3 body regions during the past 3 months. Random-effects regression models, adjusted for demographic features, depression, CWP, and familial/genetic factors, were used to examine the relationship between the IES and TMD pain.
Results: IES scores were significantly associated with TMD pain (P < .01). Twins in the highest IES tercile were almost 3 times more likely than those in the lowest tercile to report TMD pain, even after controlling for demographic factors, depression, and CWP. After adjustment for familial and genetic factors, the association of IES scores with TMD pain remained significant in dizygotic twins (Ptrend = .03) but was not significant in monozygotic twins (Ptrend = .30).
Conclusion: Post-traumatic stress disorder symptoms are strongly linked to TMD pain. This association could be partially explained by genetic vulnerability to both conditions but is not related to the presence of CWP. Future research is needed to understand the temporal association of PTSD and TMD pain and the genetic and physiological underpinnings of this relationship.J Orofac Pain 2008;22:41–49
As indicated in the study, stress can lead to TMJ disorders among other health conditions. At AZ TMJ, we not only treat the pain, but help our patients find ways to make positive life changes in order to cope with stressful periods. We focus on non-surgical and non-narcotic treatment methods. Dr. Stan Farrell is Board Certified in Orofacial Pain and has extensive training in the treatment of TMJ disorders and migraine headaches. If you feel your stress may be causing you TMJ pain or headaches, call and schedule an appointment with Dr. Farrell at 480-945-3629. www.headpaininstitute.com